

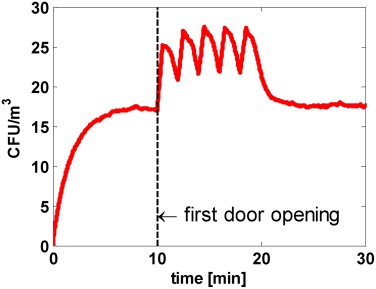
Contamination comes from nearly every staff activity in the OR: changing gowns1 and gloves2, walking around3, shedding squames4, opening doors5, applying stockinettes6, etc. This bacteria becomes airborne and is a leading cause of Surgical Site Infections (SSIs)7.
These unavoidable activities necessitate disinfection during surgery, something that terminal cleaning alone cannot provide.





Zener is a patented device, the size of a smoke alarm, that is ceiling-mounted and can increase operating room (OR) air changes by 80%8.
Zener uses SafeRayTM light technology (222 nm far-UV) which has proven to be as effective as traditional UV light at disinfection, but is safe for human exposure. This unique differentiator allows Zener to provide high bactericidal efficacy pre-, intra-, and post-operatively.
Until 2010’s, some facilities used traditional UV light (the harmful kind) in a similar manner i.e. in OR ceilings to disinfect during surgery.
With statistically significant reduction in SSIs, the efficacy was irrefutable:
However, despite the high effectiveness, the practice did not become widely adopted due to safety concerns and staff injuries from the harmful UV.
With SafeRay light’s safety differentiator and equivalent disinfection to traditional UV light8, the same application in OR ceilings during surgery is expected to offer similar SSI reduction (81% avg.) but without staff injuries.

1 Bible, Jesse E et al. “Which regions of the operating gown should be considered most sterile?.” Clinical orthopaedics and related research vol. 467,3 (2009): 825-30. doi:10.1007/s11999-008-0341-1.
2 Kim, Katy et al. “Glove change to reduce the risk of surgical site infection or prosthetic joint infection in arthroplasty surgeries: a systematic review.” ANZ journal of surgery vol. 89,9 (2019): 1009-1015. doi:10.1111/ans.14936.
3 Sunagawa, S et al. “Airborne particle dispersion around the feet of surgical staff while walking in and out of a bio-clean operating theatre.” The Journal of hospital infection vol. 106,2 (2020): 318-324. doi:10.1016/j.jhin.2020.07.016.
4 Wernham, A G et al. “Effect of an exfoliating skincare regimen on the numbers of epithelial squames on the skin of operating theatre staff, studied by surface microscopy.” The Journal of hospital infection vol. 100,2 (2018): 190-194. doi:10.1016/j.jhin.2018.03.014.
5 Sadrizadeh, Sasan et al. “Airborne particle dispersion to an operating room environment during sliding and hinged door opening.” Journal of infection and public health vol. 11,5 (2018): 631-635. doi:10.1016/j.jiph.2018.02.007.
6 Noguchi, Chieko et al. “Factors contributing to airborne particle dispersal in the operating room.” BMC surgery vol. 17,1 78. 6 Jul. 2017, doi:10.1186/s12893-017-0275-1.
7 Gosden, P E et al. “Importance of air quality and related factors in the prevention of infection in orthopaedic implant surgery.” The Journal of hospital infection vol. 39,3 (1998): 173-80. doi:10.1016/s0195-6701(98)90255-9.
8 Zener’s third-party testing to standards ANSI/AHAM AC-5, ASHRAE 241, and FDA GLP. 23 Apr. 2025.
9 Eadie, Ewan et al. “Far-UVC (222 nm) efficiently inactivates an airborne pathogen in a room-sized chamber.” Scientific reports vol. 12,1 4373. 23 Mar. 2022, doi:10.1038/s41598-022-08462-z.
10 Ritter, Merrill A et al. “Ultraviolet lighting during orthopaedic surgery and the rate of infection.” The Journal of bone and joint surgery. American volume vol. 89,9 (2007): 1935-40. doi:10.2106/JBJS.F.01037.
11 Lowell, J D et al. “Ultraviolet radiation and reduction of deep wound infection following hip and knee arthroplasty.” Annals of the New York Academy of Sciences vol. 353 (1980): 285-93. doi:10.1111/j.1749-6632.1980.tb18931.x.
12 Wright, R. Lewis, and John F. Burke. “Effect of Ultraviolet Radiation on Post-operative Neurosurgical Sepsis.” Journal of Neurosurgery, vol. 31, no. 5, Nov. 1969, pp. 533–537. https://doi.org/10.3171/jns.1969.31.5.0533.
13 Hart, D. “Bactericidal ultraviolet radiation in the operating room. Twenty-nine-year study for control of infections.” Journal of the American Medical Association vol. 172 (1960): 1019-28. doi:10.1001/jama.1960.03020100027006.
14 Overholt, Richard H., and Reeve H. Betts. “A Comparative Report on Infection of Thoracoplasty Wounds: Experiences with Ultraviolet Irradiation of Operating Room Air.” Journal of Thoracic Surgery, vol. 9, no. 5, June 1940, pp. 520–529. https://doi.org/10.1016/S0096-5588(20)32260-1
15 Kapadia, Bhaveen H et al. “The economic impact of periprosthetic infections following total knee arthroplasty at a specialized tertiary-care center.” The Journal of arthroplasty vol. 29,5 (2014): 929-32. doi:10.1016/j.arth.2013.09.017.